Temporomandibular joint disorder
Case study
A woman having undergone a major surgery under general anesthesia in October 2008 (general anesthesia also means intubation) developed constant pain in the left temple in the month following the surgery that may correspond to a temporomandular joint disorder. She consulted her family physician and her optometrist and they found nothing abnormal.
In September 2009, the pain was so intense that she lost consciousness at work. She is a receptionist.
At the emergency room, trigeminal neuralgia is suspected and a consultation to the Montreal Migraine Clinic is recommended.
Trigeminal neuralgia:
• Pain in the head and face striking acutely (paroxysmal) and briefly along the area of innervation of the trigeminal nerve.
• Would be triggered by the compression of the nervous branches by adjacent blood vessels (arteries), but decompression does not relieve the pain in all patients.
• Carbamazepine is a pain killer and anticonvulsant used in the treatment of trigeminal neuralgia. Side effects of this medication include drowsiness, ataxia, nausea and anemia. A complete blood formula must be obtained before, during and after therapy.
However, the Migraine Clinic diagnoses a Horton cephalalgia (vascular facial algia or cluster headache). This diagnosis ended up being false afterwards as the hemicrania continued (paroxysmal hemicrania).
Cluster headache (vascular facial algia):
• Unilateral (appearing on one side only), acute and intense pain located in the orbital, supraorbital and/or temporal areas lasting 15 to 180 minutes and occurring once every 2 days or up to 8 times per day.
• The attacks occur in series during weeks or months separated by remission periods.
• To confirm such diagnosis, at least 5 attacks must have occurred.
• 100% of individuals having this type of migraine either have tooth pain (53%) or jaw pain (47%).
• This disorder mainly occurs in men in a M:F ratio of 6:1. The prevalence within the population is estimated to 0.005% to 0.24% and occurs during the third decade of age (the thirties).
• Home oxygen therapy would be efficient in the treatment of this type of headache. Consult the document of the Agence d’évaluation des technologies et des modes d’intervention en santé (AETMIS): Horton cephalalgia (in French).
Paroxysmal hemicrania:
• Similar signs and symptoms of the vascular facial algia, but lasting a shorter period of time.
• 70% of affected individuals are women in their thirties.
• We can observe up to 15 attacks in a 24-hour period of a duration of 5 to 20 minutes.
• Indomethacin is extremely efficient (12.5 to 250 mg/day).
A consultation in neurology at the Notre-Dame Hospital in December 2009 brings more precision. Cervicogenic headaches following bad intubation (or laborious intubation) are mentioned.
Taking Lyrica, efficient in neuropathies associated with post-zoster neuralgia (ref: herpes zoster virus causing shingles) was not efficient. Topamax, indicated in migraine prophylaxis in adults, ended up being as inefficient with this patient.
A scan and X-ray showed the presence of 3 cervical hernias. An orthopaedic surgeon performed a facet block that removed the formication in the arms during 2 months, but not the pain in the left temple. In September 2010, the orthopaedist prescribed a cervical epidural injection and the patient took carbamazepine for 6 months. The pain was reduced, but it was always present.
Cervicogenic headache:
• Pain referred to any part of the head where the nociceptive (pain) origin comes from musculoskeletal tissues innervated by cervical nerves going through cervical vertebrae.
• These headaches are moderately severe, diffuse, unilateral (left or right), but do not change sides; in other words, they do not start on the left to end up on the right.
• These headaches can last for 1 to 3 days and come with multiple symptoms including watering of the eye, conjunctival hyperemia, dizziness, nausea, vomiting, hypersensitivity to light or sound.
• The three first cervical nerves are most often involved and interact with V (trigeminal), VII (facial), IX (glossopharyngeal), X (vagus), XI (accessory or spinal-accessory) cranial nerves. See this document: Céphalées, vertiges et rachis cervical (in French).
So in the fall of 2010, the pain was reduced, but present. In May 2011, Marie’s dentist detected cracked teeth and recommended an occlusal splint. She was referred to another dentist who recommended an MRI which put in evidence that the left articular disc was perforated. An occlusal splint was made, muscle relaxants and anti-inflammatory drugs were prescribed.
Wearing the splint caused pain in the side of the face and in the temple on the first night.
Here is thus the summary of Marie’s story that we find on Dr Jules Lemay’s site by following this link (in French).
Since Dr Jules Lemay asked me what I thought about this case, I thus provided a first response (in French) where I try to reason the clues that Marie gives us.
What can we understand and conclude?
First, the clues:
A major surgery under general anesthesia.
Working as a receptionist that leads to holding a telephone receiver between the shoulder and the head or using a headset which can apply pressure on the temples (depending on the headset model).
Three (3) cervical hernias.
Formication in the arms disappeared after a facet block.
Modifications to teeth: cracked enamel. This could be a probable consequence of bruxism (teeth grinding) or clenching.
A perforated articular disc (or it is the retrodiscal ligament band and the disc is anteriorly compressed).
Impression and conduct
I recognize that wearing an occlusal splint is efficient in decreasing the number of episodes of jaw clenching and relieving muscular pain triggered by these episodes. It is also indicated in cases of disc dislocation with or without reduction.
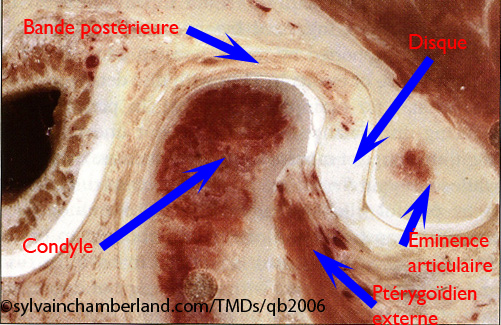
Internal derangement of the TMJ. The articular disc is blocked anteriorly from the condyle. The retrodiscal ligament band acts as a disc, but it is not designed for this function. Source: TMDs. An evidence-based approach to diagnosis and treatment, Laskin et al, Qb 2006.
In Marie’s case, a disc dislocation without reduction probably occurred and could be linked to intubation during the general anesthesia, but several people suffer from disc dislocations without having undergone general anesthesia like several people who undergo general anesthesia do not suffer from disc dislocation afterwards.
Regardless, Marie recuperated from this dislocation and was able to open her mouth about as wide as 40 mm. Let’s note that the pain increases between 20 and 40 mm of opening, which indicates that the disc probably stayed blocked and that the joint works on the retrodiscal band that stabilizes the disc on the head of the condyle if it is not dislocated, but that was stretched following dislocation. Episodes of clenching or bruxism could have contributed to the perforation of the retrodiscal band.
Is it a temporomandibular disorder?
I invited Marie not to have a reductive vision of her state and pretend that her problems were coming uniquely from her occlusion or from her TMJ.
It would be the same as pretending that the Earth is at the centre of the universe.
I believe that the cervical hernias were underestimated in Marie’s problems in the way that a consultation or physiotherapy treatments could have or should have been prescribed. Moreover, a consultation in ergotherapy to evaluate the working posture would not be unnecessary.

Nociceptive innervation from the neck to the face
On the right image, it is described that a painful stimulation coming from C3 converges on the trigeminal neuron creating a nociceptive (pain) input ascending onto (toward) the cerebral cortex. This input is perceived in the cortex as being pain in the cervical regions and TMJ even if this input originates uniquely from the cervical region.
In simple terms, injury to the C2-C3 region (intervertebral nerve) triggers pain referred to the angle of the lower jaw (mandibular angle), to the temporomandibular joint and to the temple (region of the temporal muscle).
Injury to the C2 region triggers diffuse pain in the suboccipital, occipital and frontal regions.
Injury to the C4 region can cause losses in sensitivity, numbness in the arms and hands.
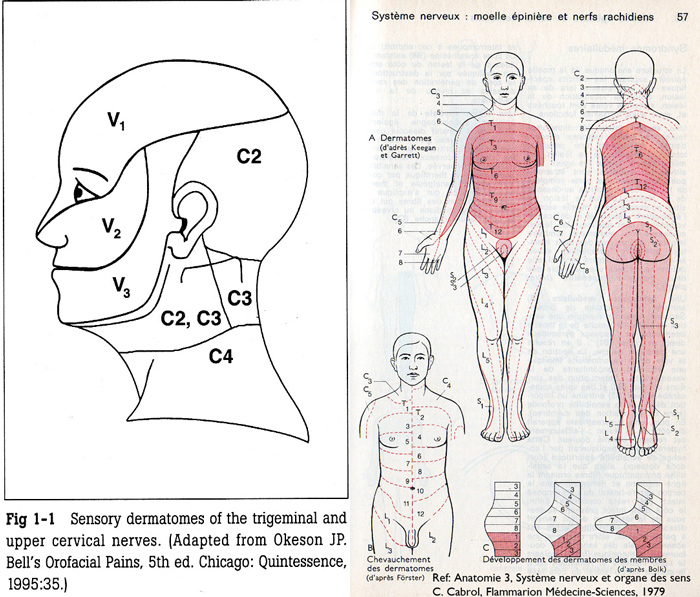
Dermatomes of the head and neck
Dermatomes (area of skin innervated by a nerve coming from the spinal cord) show that cervical nerves from C2 to C7 innervate the head and the upper limbs (arms). Marie’s cervical hernias (there are 3 of them) probably affect vertebrae below C3, because a facet block decreased formication in the arms. This means that nerves C4, C5 or C6 are affected.
Recommendations
I recommend that Marie consults a certified physiotherapist. The evaluation of cervicothoracic junction injuries is necessary. Specific exercises guided by a kynesiologist to strengthen the cervical and back muscle structure can only be beneficial.

Bad working posture of a medical technologist. The posture can be similar to the one of a receptionist seated at a front desk. The arrows represent the zones of constraining postures on the arms, shoulders and neck.
Consult an ergotherapist to evaluate the working posture. As an example, the Association paritaire pour la santé et la sécurité du travail du secteur des affaires sociales published a prevention guide on musculoskeletal disorders in dental clinic (www.asstsas.qc.ca). Reference: Prevention action leaflet: Pipetter en sécurité pour prévenir les TMS chez les technologues (in French)
Continue the use of the occlusal splint, but do not believe that this will resolve your headache problems totally, because the cause is very likely elsewhere (cervical spine).
If no convincing results occur within the following 3 months, ask yourself some questions. It is a little like medication that you have taken which has not cured anything.
If it doesn’t work, it means it is not the right treatment.
Worse, if it works, it does not even mean that your disc and your TMJ were causing your headache problems. They were maybe only the effect of another problem.
I do not recommend any irreversible TMJ surgical procedure at this point.
I recommend an evaluation by an oral surgeon (Dr Dany Morais or Dr Carl Bouchard) for the joint condition and an orthodontist for the occlusal condition (the dentition).
References:
TMDs: an evidence-based approach to diagnosis and treatment, Laskin D. M., Green C. S., Hylander W. L., Qintessence book, 2006
Orofacial Pain, from basic science to clinical management, Lund J.P., Lavigne G.J., Bubner R., Sessle B.J. Quintescence book, 2001
Orofacial Pain, from basic science to clinical management 2nd edition, Lund J.P., Lavigne G.J., Bubner R., Sessle B.J. Quintescence book, 2008
Orofacial Pain, guidelines for assessment, diagnosis and Management, edited by Jeffrey P. Okeson et coll, Quintescence book, 1996
Orofacial Pain, guidelines for assessment, diagnosis and Management, 4th edition, edited by Reny de Leeuw et coll, Quintescence book, 2008

Dear Dr. Chamberland,
I would greatly appreciate your professional advice on my complex case.
I developed tmd 6 months ago with symptoms of clicking/popping when swallowing, ROM 32-35mm, difficulty chewing properly, sometimes even difficulty swallowing and talking. I have a deep overjet and overbite which seems to have gotten worse. My occlusion is completely off as I have no teeth contact except for one molar. I had an MRI and was diagnosed with mild anteromedial displacement with a bit of left condyle flattening but was told my joints are adaptive. I have consulted with several dentists, 4 orthos and oral surgeon but I’m not sure which is the best approach for treatment based on my case. My main concern is finding optimal jaw position and fixing my bite. I’m from the Toronto area, do you know of any specialist who has expert knowledge in tmd and malocclusion? Thanks in advance!
There excellent orthodontist in Toronto and most of them can manage your case. I can name some, but there would be too many. It would be very helpfull if you could tell me in which area of Toronto you live and I will ask a friend if he can recommend 1 or 2 names. My concerns is that you already met 4 orthodontists. I would be surprise if there opinion would be very different from one another. The same would apply to the oral surgeon you met.
You can write their name in you reply. I WILL NOT publish their name ( I am the only moderator of this blog) and may tell you i know this one or the other, but it would not mean that those I don’t know are not good.
I hope that help.
Thanks for your response. I am from the North York area of Toronto. The 2 orthodontist I saw weren’t experienced with tmd whereas the other 2 I saw were Dr. B and Dr. R. There was some variation of treatment options including braces and jaw surgery to conservative management of tmj first prior to braces. I am concerned about starting braces with preexisting tmj and it possibly making my tmj symptoms worse. However, I know leaving my maloclussion the way it is could further make my tmj worse. How do you approach treating your patients with braces if they have tmj?
It make sense to do conservative treatment prior to surgery. However, I don’t know the nature of your TMJ problem. Is it a degenerative problem?
I ask to a friend of TOronto. He said that Dr B is good with TMJ.. He don’t know about Dr R. This does not that Dr R is not good. It mean that my friend simly don’t know about him.
Listen to your feeling. Chose the one you are confident with.
I can not tell you which one to go.