Orthognathic surgery
Indications
Orthognathic surgery is indicated when a patient has an orthodontic problem sufficiently severe to conclude that compensation or concealment treatments are no longer treatment solutions. A surgery to realign the jaws or reposition dentoalveolar segments then becomes the only possible treatment.
The surgery is not a substitute for orthodontic treatment. It is part of the orthodontic treatment and must be coordinated with it and with other restoration treatments (implants, prosthodontics, periodontics) if required.
Contemporary surgical techniques
Maxillary surgery
• Surgically assisted rapid palatal expansion (SARPE)
• Le Fort II and Le Fort III osteotomies (these two procedures are less common and are generally reserved to craniofacial syndromes, such as Crouzon and Apert).
Mandibular surgery
• Bilateral sagittal split osteotomy (BSSO)
Distraction osteogenesis
This type of surgery is based on the principle of manipulation of the cutting site of the bone to stretch the blood clot that forms to repair the site before this clot (soft callus) is remineralized and reossified. Among the benefits of distraction osteogenesis, we note that movements of greater amplitude can be executed and that deficient jaws can be lengthened at a younger age. We can then lengthen or widen a maxilla or mandible by using this technique.
SARPE is based on the principle of distraction osteogenesis.
It is possible to widen the mandible at the chin level by symphyseal distraction osteogenesis.
The following Keynote presents the steps of cut of Le Fort I surgeries, bilateral sagittal split osteotomy and genioplasty. The type of fixation used is presented. It is quite a succinct, but very explicit visual aid.
Hierarchy of stability

Hierarchy of stability of orthognathic surgeries. Author: Dr William Proffit.
Le Fort I osteotomy

Le Fort I osteotomy
Cut lines of the Le Fort I osteotomy are located on the lateral walls of the maxillary bone and spread anteriorly from the nasal aperture up to the pterygomaxillary junction posteriorly. This line is located above the dental roots and goes under the zygomatic arch. The internal wall of the sinus as well as the nasal septum are separated with an osteotome. The maxilla is then separated (down fracture) from the pterygoidal plates.
This type of osteotomy allows the repositioning of the maxilla in the 3 planes of space. Most frequent types of movement are advancement, upper repositioning (impaction) and lower repositioning. A combination of movements is possible: anterior and superior, anterior and inferior, rotation (anterior lowering and posterior lifting). In front view, it is possible to correct an inclination by lifting or lowering one side more than the other.

Upper maxilla partition
To correct the maxilla in width, it has to be partitioned in 2 at its middle or in 3 segments (1 anterior and 2 lateral) depending on the required expansion. The figure of the maxilla in occlusal view shows the position of the cut lines. The blue arrows show the junction of the maxilla at the pterygoidal plates of the sphenoid bone. These junctions have to be broken if the maxilla needs to be moved or widened.
Bilateral sagittal split osteotomy (BSSO)

Bilateral sagittal split osteotomy (BSSO)
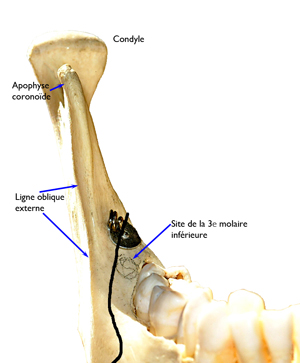
Sagittal split osteotomy consists of cutting through the mandible between the ramus and the body of the mandible (black line). This cut spreads vertically from the inferior border of the body of the mandible to the superior junction approximately between the first and second molar. This line continues posteriorly between the external oblique ridge and the teeth, up to the ramus. The line continues on the internal side of the ramus and goes above where the inferior alveolar nerve goes in.
Cut in front view
In front view, we can see the width of the body of the mandible and the path of the cut. You will recognize that the line passes across the site of the third molar. This tooth, even though it is not visible on this dry mandible, still has the same dimension as a marble of 10 to 15 mm in diameter if we include the follicular envelope that surrounds it. There is thus a cavity in the bone that, when the 2 bone parts are separated, thins down the remaining bone walls as much. This is the reason why oral surgeons prefer that the third molars be removed at least 6 months before an orthognathic surgery, because it is important to have bone walls in full width when they have to fix fragments with bicortical screws.

Bicortical screws
Bicortical screws are inserted at a right angle and immobilize the external wall against the internal wall in order for complete healing to occur. It is possible to understand, through the X-ray image, that the screws are positioned where the third molar germ should normally be located.
Genioplasty

Cutting site in genioplasty
Genioplasty can be used to correct anomalies in the anteroinferior part of the mandible border. In this regard, genioplasty is an inferior border osteotomy of the mandible and allows the modification of the edge of the chin in the 3 planes of space and change of the shape of the chin in height (vertically), in length (anteroposteriorly) and in width (transversally). Genioplasty can be executed alone or together with other maxillary or mandibular osteotomies.
The cut line is located under the apex of the root of the mandibular incisors and spreads posteriorly diagonally by going under the mental foramen where the mental nerve, which gives sensation to the skin and mucus membrane of the chin and lower lip from the labial commissure, comes out.

Osteosynthesis in genioplasty
The inferior (distal) bone part detached from the body of the mandible (proximal segment) is slid anteriorly and immobilized with metal osteosynthesis or bicortical plate and screws. The example on the left with metal osteosynthesis represents vertical reduction and advancement. The example on the right with a bicortical plate shows advancement, but very little vertical reduction. These X-rays were taken 2 weeks after the surgery.
Back to top.
Surgically assisted rapid palatal expansion (SARPE)
When an individual reaches his/her physical maturity, the orthopaedic expansion of the maxilla obtained in a growing individual is no longer possible. An expansion appliance (in adults) fixed on the teeth would only tip the teeth without expanding the basal bone.
There are two ways to expand the palate in adults:
1- Expand the palate by segmenting the maxilla during a Le Fort I osteotomy
2- Expand the palate by using the principle of distraction osteogenesis (SARPE)
SARPE is the equivalent of a Le Fort I osteotomy with the same cuts except that there is no down fracture. The cut line (white arrows) starts at the piriform (pear-shaped) aperture of the nasal cavity and spreads posteriorly up to the pterygomaxillary junction by going under the zygomatic arch where the line is widened. The 2 hemimaxillas are separated in their middle at the intermaxillary suture by a thin osteotome. An expansion appliance was previously cemented on the teeth. It is activated periop of about 1 mm.
The expansion (distraction osteogenesis) is started 5 to 7 days postop to let the blood clot organize itself into a soft callus. The distraction is done at the rate of 0.5 mm per day until the desired dimension is obtained. In the image on the opposite side, taken at the last day of expansion, notice the space of about 10 mm between both central incisors. The separation between both incisors indicates that an adequate disjunction of both hemimaxillas was performed. This freshly created space between both incisors will close progressively while the gingival fibers, which are stretched during the expansion, will go back to their normal size. Since they are attached to teeth by cementum, the teeth will then move into this empty space. The installation of brackets will complete the closing of the diastema.
To get complete and exhaustive information on SARPE, I recommend my master’s thesis on the subject entitled: Stabilité de l’expansion palatine rapide comparée à une ostéotomie Le Fort I multisegmentée (in French).
Two articles were produced and published:
Closer look at the stability of SARPE
Short-term and long-term stability of SARPE revisited (AJODO 2011; 139:815-22)
If you really wish to see a SARPE surgery and you don’t have a weak stomach, you can watch this little video. People having a weak stomach, please refrain from watching. EPRAC_SARPE videoclip of surgical technique
Back to top.
Distraction osteogenesis
Symphyseal distraction osteogenesis is indicated in cases of severe constriction of the lower jaw. It allows the expansion of the anterior part of the mandible to thus regain the space to align the dentition on one hand and for the tongue on the other hand.

Cut on dry mandible

Cut of symphysis (oral surgeon: Dr Dany Morais)
The symphysis necessitates a vertical cut in the middle of the chin. An expansion appliance with bone anchor is the ideal appliance because the dental arch is so narrow that it is impossible to put an expansion screw in. The case illustrated on the right shows the osteotomy site. An appliance using a dental anchor was used.
Distraction osteogenesis after a periop expansion of 1 mm was continued 7 days after the surgery at the rate of 0.5 mm per day until the planned expansion was obtained.

Separation after symphyseal distraction osteogenesis

Complete healing after symphyseal distraction osteogenesis
The X-ray shows the separation obtained (section between the arrowheads) between the right and left parts of the mandible by stretching of the soft callus. This section will ossify again completely and it will not show anymore once healing is completed. When ossification of the soft callus starts, the teeth can be orthodontically moved in this newly created space. The X-ray on the right was taken about 30 months after the orthodontic treatment ended.

Bone anchor expansion device (oral surgeon: Dr Dany Morais)
The example on the opposite side shows a bone and dental anchor expansion device. The space obtained by expanding the symphysis allows the alignment of teeth and allows the tongue to finally be able to move inside the dental arch. Mandibular distraction can be done simultaneously with SARPE. Mandibular expansion can be part of a major orthosurgery treatment to fix a severe obstructive sleep apnea disorder.
Scott Conley and Harry Legan published an excellent article in the AJODO in 2006 to illustrate a case of severe maxillary and mandibular constriction and mandibular retrognathia in an apneic patient. Correction of severe obstructive sleep apnea with bimaxillary transverse distraction osteogenesis and maxillomandibular advancement.
Benefits of surgery
Treatment benefits can be astonishing.
Even if the possibility of undergoing a surgery as part of your treatment plan can seem intimidating to you, it is really common. Once the orthodontic and surgical treatments are completed, you will be able to enjoy a better dental health and have a better facial appearance.



Hi I believe I may have bimax protrusion.. I am of African American decent and I know it is more common in mines and Asian races to have. And was wondering can surgery fix it ?
Bimax protrusion can be solve by 4 premolars extraction.
SUrgey may be possible if there is a skeletal discrepancy too.
Hi. Just wondering what a ball-park figure of the average cost is for SARPE surgery? Thanks.
SARPE is covered by national health care system. There is a cost, but it does not affect the patient directly. We all pay income tax for canadian health care.