Dr Sylvain Chamberland, Orthodontiste says:
First of all, an impacted canine CAN NOT cause oral cancer. Period.However, some pathology can arise from the dental follicule. The most common would be dentigerous cyst.
In my collection of oral pathology I found this:
1- Dentigerous cyst

This show an elargment of the follicule around the crown of the impacted canine.
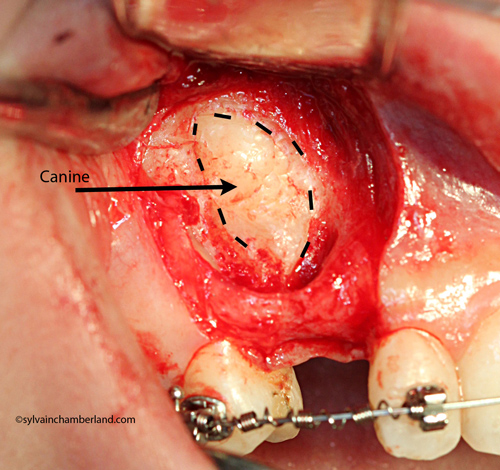
2- Central giant cell tumor
 This is an impacted canine of an 11 years old female.
This is an impacted canine of an 11 years old female.Central giant cell tumor is seen predominantly in patients under 20 years of age and occurs more commonly in females than in males, more frequent in the mandible than the maxilla, generally anterior to the 1st molar. This lesion is expansile producing a discernable enlargement and cortex destruction. It may displace adjacent teeth.
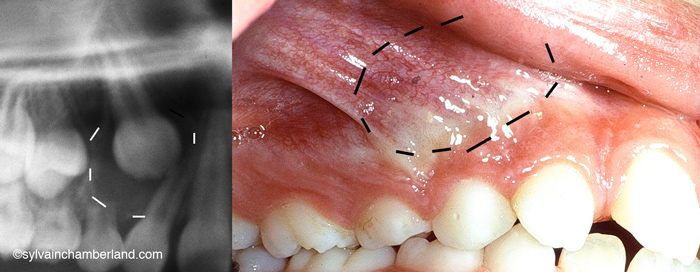
3- Odontogenic adenomatoid tumor (AOT)
 This 9 years old girl that was refered to the oral surgon for an impacted canine and deformation of the cheek.
This 9 years old girl that was refered to the oral surgon for an impacted canine and deformation of the cheek.One can see an enlarge cyst with displaced adjacent teeth involving the lateral incisors and the 2 premolars. The CBCT scan see enlargment of the cortex, displacement of the impacted canine toward the orbit.
Approximately 70% of AOT's occur in females younger thant 20 years of age and 70% involve the anterior jaw. Association with impacted canine is common. Therefore on radiograph, it can be mistaken for dentigerous cyst.
3-Root resorption
 Root resorption of teeth adjacent to an impacted canine is common. You should not take that risk lightly.
Root resorption of teeth adjacent to an impacted canine is common. You should not take that risk lightly.Conclusion
An impacted canine should not be left alone. It may cause significant problems
Baskar SN, Synopsis of Oral Pathology, Mosby, 1977
Glick M et al, Burket's Oral Medecine 12th ed. PMPH-USA, 2015