The comments
Dr Sylvain Chamberland, Orthodontiste says:
You should consult an orthodontist or at leat visit a dentist. I do not recommend extraction of the canine. You may have periodontal abcess if the tooth is partially erupted.Visit a dentist or an orthodontist.
Dr Sylvain Chamberland, Orthodontiste says:
Sorry for the delay, i forgot to verify the english version of the site.I would not us a Jasper Jumper to correct a class II div 2 in an adult female. No way it will correct the skeletal relationship. Success is very unlikely.
Your best option is surgery to advance the mandible of extraction of 2 maxillary premolar for a camouflage.
I recommend that you consult an orthodontist.
Dr Sylvain Chamberland, Orthodontiste says:
I apologies for the delay. I verify less often the english version of the site.Anchored molars may tip outward as the device is activated, but it is unlikely in a young patient. If the patient has 15-17 years old, there is more chances to have buccal tipping. The appliance should be very rigid.
I hope that help.
tiffany gruwell says:
I'm 21 years old, and was told at 13 my front right canine would never grow in. They left it, and at 18, it pushed past my other teeth and turned itself sideways. At 21, it's only halfway grown in, and is constantly swelling. Could it be infected? Does it need to be pulled? I'm not sure what to do. Thank you.Lucille says:
Hello. I am a 42 year old adult woman with a Class II malocclusion, Division 2 with severe overbite. I am thinking about receiving orthodontic care and I have heard that the use of Jasper Jumpers is a viable option for me.I am wondering about your expert opinion on this as you seem very knowledgable and I would like to know all the pros and cons of this treatment should I choose this treatment.
I think the Jasper Jumpers put a force on the maxilla that pushes it back(which seems like an easy option) and wanted to know if there any ramifications for someone like me who is a non growing adult.
It seems like it would be a viable option for someone of my age.
I have also read that surgery is an option, but if this appliance is effective, it seems to be an easier choice. If I choose to go with Jasper Jumpers, how do I find an orthodontist that has the training and knowledge to use them or what questions should I ask.
These seem to have been around a long time and wanted to know what the orthodontic community success rate for these have been with someone with my class II division 2 before I commit to treatment.
Thank you. Lucille
Matthew says:
Is it normal for the molars that are anchored by the expander to tip outwards? I was told by my orthodontist that it is normal; however, most of what I have read online says otherwise. I would appreciate your expertise.Dr Sylvain Chamberland, Orthodontiste says:
It would be much appreciated if you keep us informed.Cordialement,
Dr Sylvain Chamberland
Ellena says:
Thank you very much!Dr Sylvain Chamberland, Orthodontiste says:
I went back to the cephalogram on your website of your son's treatment and found the ceph taken on july 15, 2014. I wounder why nobody sugestted an alternate treatment plan that would have involve extraction of the ankylose canine and 3 premolars.It is quite clear from the tracing that maxillary incisors are proclined by 5° (mx1-SN = 109,4°; norms 104°), lower incisors are proclined by 14° (IMPA = 104°; norm = 90°) and interincisal angle is decreased by 15° (1/1 = 115°; norm 130°).
Extraction of the ankylosed canine and 3 premolars would have help to reduce the dentoalveolar protrusion and achieve normal class I occlusion without the burden of waitng the right age to get an implant in a cosmetic zone where it will always be a challenge to have smile esthetics.
I doubt that an autogenous transplantation would be a viable option.
I would like show you this exemple where the patient was told that the canine might be ankylosed and that extraction of 3 premolars was the best option.

My concern is that your son is into orthodontic treatment for so long and closing the space os canine and premolar extraction means 12 to 18 more months of treatment. It is sad that nobody has thought about an alternate treatment plan earlier.
Dr Sylvain Chamberland, Orthodontiste says:
Timing is critical when you plan to extract all first molars to close an open bite. It should be done before the eruption of the 7s. The disadvantage is that the vertical growth pattern continue and the bite may reopen after ortho treatment.If you extract 1st molar in a high angle case that has no open bite and the premolar are in occlusion, it will not have any effect on the vertical dimension.
Dr Sylvain Chamberland, Orthodontiste says:
Progressive condylar resorption
You have a good question. Is it possible to have a condylar resorption AND a deep bite? I don't recall in any of the cases I have seen, and I have quite quite a fair number, that thse 2 conditions coexist.
Is someone have condylar resorption, the ramus become shorter and a the bite will likely open anteriorely with fulcrum at the 1st-2nd molar area.
The surgeon might be right when he say you don't have CR because your don't have a high mandibular plane angle and you have a deep bite. A simple panoramic xray can provide good information on the possibility of having condylar resorption. If so, then a CBCT scan of your TMJs would be the next imaging I would recommend. A MRI is a good imaging approach, but studies have shown that the sensitivity is 78% and the predictive value is only 54%.
The key factor is do you have pain? Did the ovejet increased recently? Did you had a bone scan to asses if you have bone remodeling activities?
If you can send me a panoramic xray via my professional facebook page, I could give you an opinion.
Dr Sylvain Chamberland, Orthodontiste says:
I finally remembered a name of a famous oral surgeon from Pretoria, South Africa. He has written texbooks that the residents in oral and maxillofacial surgery used here in the program of Maxillofacial surgery of Hôpital l'Enfant-Jésus.Therefore, I would receommend you Prof. JP Reyneke or any member of his team, Dr van der Linden or De Beukes. Their website is minimalist but Dr Reyneme's textbook is excellent.
Dr Sylvain Chamberland, Orthodontiste says:
Canine exposure and perio packing
Yes.
You can see at the beginning of this page a case from a collegue in Ontario. This is a good exemple of healing with a perio packing.
The goal of a perio packing is to obtain healing of the palatal mucosa without recovering the impacted canine. Ususally, I removed the perio packing 10 to 14 days after the surgery and I initiate immediately the orthonontic traction qith either a removable or a fixed appliance.

In this case, when the patient came, it might be 7-10 days after surgery. I removed the packing and i was ready to intiate the traction because the surgeon had bonded a button and attached a wired ligature.
The follow up of this case show a good healing and the canine remain visible, not covered by gingival tissue at 2 and 4 monhts.
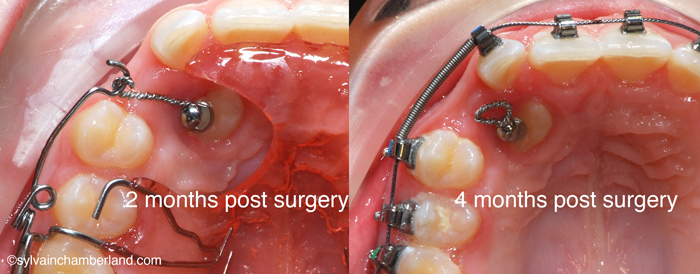
At 4 months into treatment, I had to change the biomechanic. Theferore i used fixed appliances from this moment.
BL says:
Also, in regard to the Tc 99 bone scan - I've been reading about it online, but I'm not quite sure what to ask for.Is it standard for most radiologists know about the uptake in the condyles and what to compare the ratio to? Or would I have to get my referring doctor to specifically provide the details such as standard levels/specify the other area of the body to compare to?
Is this only done through a SPECT scan?
I am in Australia and there is barely any information about local cases of CR, so while we have SPECT scans, I'm unsure if this actual scan is ever done in relation to CR.
Abbas says:
Hi great article to read, am 1st year post graduation student,Whats your experience on effect of all first molar extraction on vertical dimension in high angle case.
Warm Regards
Abbas
BL says:
Dr. Chamberland, thank you very much for sharing your slide-show presentation. It has been very informative.My problem started 10 years ago at age 22, with pain in one side. A CT scan showed degenerative changes in both condyles, but one side worse than the other. I also developed an overjet.
I didn't seek/continue any treatment, besides a short time in a splint, as my pain went away, and the only problem was my overjet/protruding incisors. I assumed they could be treated orthodonticaly in the future.
Since 3-4 yrs ago I noticed my face and profile looking different. My lower jaw seems to be sitting further back and I feel I have extra skin under my chin/neck area. My overjet is 9mm.
This year I decided to investigate getting braces. I was referred to assess the health of my TMJs, and had a MRI recently that reported 'severe osteoarthritis of both temporomandibular joints compatible with degeneration, tearing and resorption'.
My situation is slightly different though: I don't have an open-bite. Rather, my bite has been getting deeper. I apparently don't have a high-mandibular plane either. So it seems my jaw is going back, but not rotating down. Have you seen/heard of CR presenting this way before?
One surgeon told me I don't have CR because I don't have the open bite and high angle.
Can the mandible go back in just osteoarthritis, not CR? I am confused as to what I have.
I have come across only one article that mentions a deep bite:
Int J Oral Maxillofac Surg. 1999 Dec;28(6):411-8.
Long-term evaluation of patients with progressive condylar resorption following orthognathic surgery.
Hoppenreijs TJ1, Stoelinga PJ, Grace KL, Robben CM.
Any input would be greatly appreciated, thank you.
Best regards
Ellena says:
Hi DocterSome feedback: I saw the specialized scans of my joints. I need a TMJ replacement on the one side.
It does not appear to be related to condylar resorption. The fracture (split diagonal below the condyle) from an earlier 'complication' during orthognactic surgery has not closed as the bone didn't make contact. This has left my jaw very unstable.
My problem now is finding the right surgeon.
Thank you again for your kind assistance.
Regards
Ellena
Michael B. says:
Dear Dr. Chamberland,My son had the procedure to remove 4 baby teeth and expose the canines on the palate side. They are impacted. This was 1.5-2 months ago. The perio packing has now fallen out on both sides while eating cheerios and a toasted roll. Is the normal? After 2 trips to repair one side then the other, it happened again. The surgeon now say to go back to the orthodontist because the teeth may be erupting. Do you think the exposure procedure can work in just 2 months?
Thank you
Michael